The study involved five major activities to estimate the current size of the Medical Billing market. Exhaustive secondary research collected information on the market and its different subsegments. The next step was to validate these findings, assumptions, and sizing with industry experts across the value chain through primary research. Both top-down and bottom-up approaches were employed to estimate the complete market size. Thereafter, market breakdown and data triangulation procedures were used to estimate the market size of the segments and subsegments.
Secondary Research
In the secondary research process, various secondary sources such as annual reports, press releases & investor presentations of companies, white papers, certified publications, articles by recognized authors, gold-standard & silver-standard websites, regulatory bodies, and databases (such as D&B Hoovers, Bloomberg Business, and Factiva) were referred to to identify and collect information for the study of Medical Billing Market. It was also used to obtain important information about the top players, market classification, and segmentation according to industry trends to the bottom-most level, geographic markets, and key developments related to the market. A database of the key industry leaders was also prepared using secondary research.
Primary Research
Extensive primary research was conducted after acquiring basic knowledge about the global Medical Billing market scenario through secondary research. Several primary interviews were conducted with market experts from both the demand side (Hospital directors, Hospital Vice Presidents, Department heads, and Critical care specialists ) and supply side (such as C-level and D-level executives, technology experts, product managers, marketing and sales managers, among others) across five major regions—North America, Europe, the Asia Pacific, Latin America, Middle East, and Africa. This primary data was collected through questionnaires, e-mails, online surveys, personal interviews, and telephonic interviews
The following is a breakdown of the primary respondents:
Breakdown of Primary Participants:
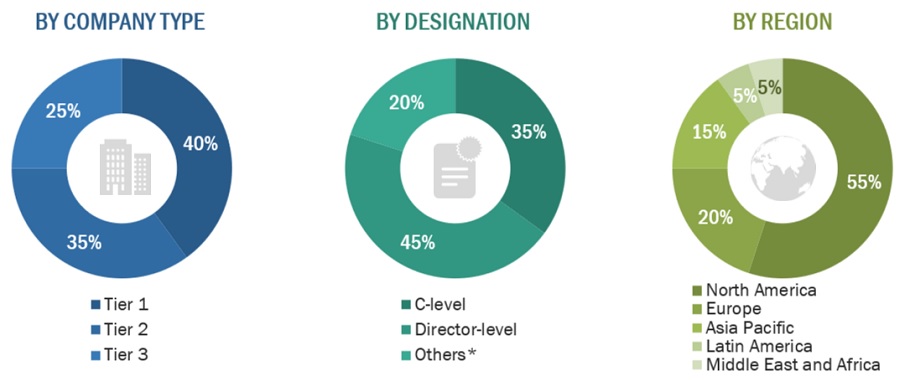
Note 1: Others include sales, marketing, and product managers.
Note 2: Tiers of companies are defined based on their total revenues in 2023. Tier 1 = >USD 1 billion, Tier 2 = USD 500 million to USD 1 billion, and Tier 3 = <USD 500 million.
To know about the assumptions considered for the study, download the pdf brochure
Market Size Estimation
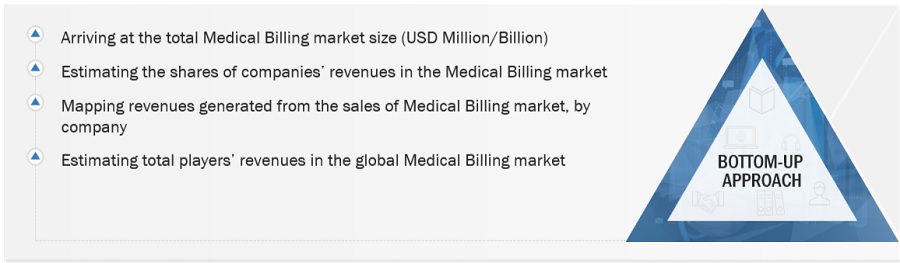
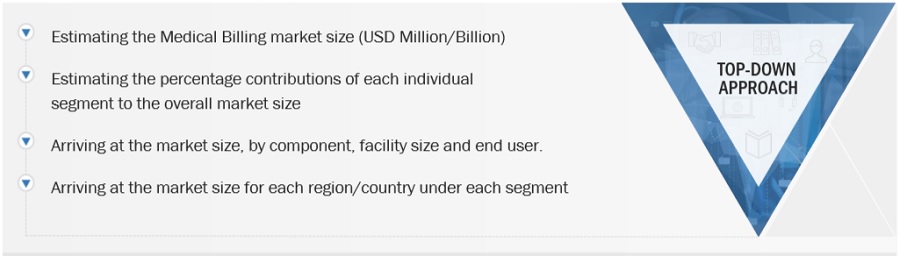
Both top-down and bottom-up approaches were used to estimate and validate the total size of the Medical Billing market. These methods were also used extensively to estimate the size of various subsegments in the market. The research methodology used to estimate the market size includes the following:
-
The key players in the industry and markets have been identified through extensive secondary research.
-
In terms of value, the industry’s supply chain and market size have been determined through primary and secondary research processes.
-
All percentage shares, splits, and breakdowns have been determined using secondary sources and verified through primary sources.
Global Medical Billing Market Size: Bottom-Up Approach
To know about the assumptions considered for the study, Request for Free Sample Report
Global Medical Billing Market Size: Top-Down Approach
Data Triangulation
After arriving at the overall market size—using the market size estimation processes—the market was split into several segments and subsegments. To complete the overall market engineering process and arrive at the exact statistics of each market segment and sub-segment, the data triangulation and market breakdown procedures were employed, wherever applicable. The data was triangulated by studying various factors and trends from both the demand and supply sides in the Medical Billing market.
Market Definition:
Medical billing is the process of creating healthcare claims to be submitted to insurance companies to get payment for medical services provided by providers and provider groups. The medical biller converts a healthcare service into a billing claim and then monitors the claim to make sure the organization is paid for the provider's work. A medical practice or healthcare organization can maximize revenue performance with the help of an experienced medical biller.
Key Stakeholders:
-
Medical Billing Vendors
-
Government Bodies
-
Healthcare Service Providers
-
Clinical/Physician Centers
-
Healthcare Professionals
-
Health IT service Providers
-
Healthcare Associations/Institutes
-
Ambulatory Care Centers
-
Venture Capitalists
-
Distributors And Resellers
-
Maintenance And Support Service Providers
-
Integration Service Providers
-
Healthcare Payers
-
Advocacy Groups
-
Data Security And Privacy Experts
-
Investors And Financial Institutions
-
Industry Associations And Trade Groups
Report Objectives
-
To define, describe, and forecast the global Medical Billing market based on component, facility size, end user, and region.
-
To provide detailed information regarding the major factors (such as drivers, restraints, opportunities, and challenges) influencing the market growth
-
To strategically analyze micro-markets with respect to individual growth trends, prospects, and contributions to the overall medical billing market
-
To analyze opportunities in the market for stakeholders and provide details of the competitive landscape for market leaders.
-
To strategically analyze the market structure profile the key players of the medical billing market and comprehensively analyze their core competencies.
-
To forecast the size of the market segments with respect to five regions: North America, Europe, Asia Pacific, Latin America, and the Middle East & Africa.
-
To track and analyze competitive developments such as product launches and enhancements and investments, partnerships, collaborations, acquisitions, expansions, agreements, sales contracts, and alliances in the Medical Billing market during the forecast period.
Available Customizations:
With the given market data, MarketsandMarkets offers customizations to meet the company’s specific needs. The following customization options are available for the report:
-
Product Analysis: Product matrix, which gives a detailed comparison of the product portfolios of each company.
-
Geographic Analysis: Further breakdown of Latin American Medical Billing into specific countries, the Middle East and Africa Medical Billing into specific countries, and further breakdown of European Medical Billing into specific countries.



Growth opportunities and latent adjacency in Medical Billing Market